Some gut bacteria can collaborate to promote T-cell action against tumours in mice, raising hopes for treatments.
A new study led by Zhejiang University researchers has identified ways by which some microbes might influence cancer immunotherapy, suggesting a potential microbial-based adjuvant approach to improve the responsiveness of immunotherapy. Their results were published in Cell1 in March 2024.
Doctors and scientists have long been puzzled about why some patients respond better than others to treatments. That’s especially the case for a new wave of cancer therapies that aim to harness the power of the body’s own immune system to fight tumours. The effects of such immunotherapy can vary widely, even between patients with similar cancers.
One possible reason is the impact of bacteria in the gut and other organs. Long considered passive passengers, these microbes are now thought to play a significant role in many physiological processes.
“The gut microbiome can influence the efficacy of immunotherapy, but the specific bacterial components and underlying mechanisms remain elusive,” says WANG Liangjing, a professor of internal medicine at the Second Affiliated Hospital at the School of Medicine, Zhejiang University.
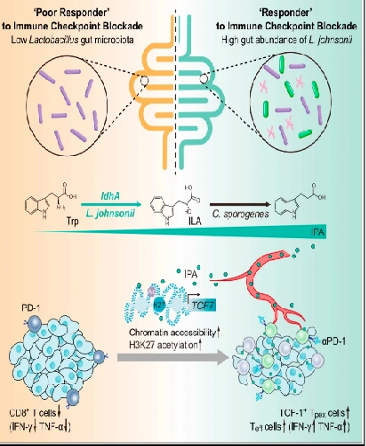
His team investigated components of the microbiome, and revealed the beneficial effects of the bacteria Lactobacillus johnsonii and Clostridium sporogenes.
Mouse model
The mouse study looked at how the two bacteria worked together to produce a chemical called indole-3-propionic acid (IPA). This is important because IPA changes the behavior of T-cells, the immune cells that are often targeted in cancer immunotherapy.
Specifically, the IPA was found to boost the so-called ‘stemness’ of the T-cells, a term used to describe their stem cell-like behavior, including self-renewal and capacity to differentiate into different types of cell. This improved their responsiveness to treatments called immune checkpoint blockade (ICB) therapies in several types of cancer.
The team then looked at whether IPA might also be able to improve the response to ICB therapies in human cancer patients. They tested this approach in vitro, using human T-cells in the lab, and found they were better able to target tumours and express helpful proteins when exposed to IPA.
“Collectively, these results demonstrate that modulating the stemness programme of T-cells through microbiota-derived IPA may be a promising approach to reinforce the effectiveness of tumour ICB therapy in clinical settings,” WANG says.
New trials
The research also produced some surprising results. The scientists could not detect IPA in the medium in which they grew the Lactobacillus johnsonii bacteria. That could indicate the microbe needs to collaborate with others to produce the target chemical.
WANG says they are now working to confirm exactly how the IPA enables the useful modification of the T-cells. The team is also carrying out trials to explore how the presence of other bacteria could boost immunotherapy further in several cancers.
As the effects of IPA on immune response are consistent across multiple cancer types, WANG says it could suggest broad “pan-cancer” applications for the approach.
“We’re hopeful that gut microbiota and microbial metabolites will shine in the process of adjuvant tumour immunotherapy,” WANG adds.
Reference
1. Wang, L. et al. Cell 187, 1–15 (2024).